From March 4 to 6 2018, we ran a workshop in Hanoi — together with Vietnam’s National Institutes for Hygiene and Epidemiology (NIHE) — on the epidemiology and evolution of influenza virus in Vietnam. The workshop summarized the past 10 years of OUCRU-led and NIHE-led studies, whose aim was to determine the patterns of persistence, seasonality, and attack rates of influenza virus in Vietnam. Additional workshop goals included an assessment of the total influenza hospital burden, and the scale at which influenza virus evolution could be observed in Vietnam. The workshop included 41 participants, 11 of whom were international and 19 of whom were speakers. Twelve ministry-level officials attended from the Vietnamese Ministry of Health, including Dr Dang Duc Anh (Director of NIHE) and Prof Le Thi Quynh Mai (vice-Director of NIHE). Prof Kanta Subbarao — Director of the WHO Collaborating Centre for Reference and Research on Influenza in Melbourne Australia — attended the workshop and gave a presentation on the WHO’s global network for influenza surveillance.
Some of the key discussion points and results from the workshop were that:
1. There is no clear influenza season in any region of Vietnam. This is important because timing of influenza vaccination has been put forward by WHO as a potential regional vaccination strategy in tropical countries. Both national surveillance data as well as mHealth data on ILI cases support the lack of any consistent influenza season in Vietnam.
2. Year‐round influenza persistence appears to be well accepted. Based on phylogenetic data, syndromic reporting data, seroepidemiological data, and literature from neighboring countries, the evidence consistently supports an epidemiogical model where influenza virus transmission is persistent and year-round in Vietnam.
3. Nationally-recommended influenza vaccination is still many years away. Influenza vaccine considerations in Vietnam would need to start with safety studies carried out in Vietnam. These studies would need to start with a (small) safety study in pregnancy, and then proceed to larger community-sized studies to assess effects on burden and seroincidence. Hospitalization data and health burden data would need to be systematically collected to determine the economic benefits of deploying influenza vaccination. Vietnam is ideally suited to attempt a school-age influenza vaccination program. This option could possibly be the simplest, least expensive, and most effective. However, this is a question to discuss in the 2020s.
4. New methodologies for attack‐rate estimates were developed. These were necessary, as we do not know during what months an influenza epidemic should occur in Vietnam, which means it is
almost impossible to take a serological cross-section after an epidemic and compute the attack rate based on this single cross-section. The new methods do not require knowledge of an epidemic’s
occurrence (either past or anticipated). They suggest that influenza A/H3N2 annual attack rates in Vietnam range from 15% to 30% in typical, non-drift, H3N2 epidemic years.
Thanks very much to Wellcome Trust and Penn State for funding the workshop. Some pictures and descriptions follow below.

Prof Kanta Subbarao, Director of the WHO Collaborating Centre in Melbourne, discussing the WHO’s global influenza surveillance system.
Prof Marion Koopmans giving a background talk on the Erasmus Medical Centre’s efforts to deploy accurate clinical surveillance systems in outbreak situations.
Dr Pham Quang Thai, vice-head of epidemiology at NIHE and former OUCRU PhD Student, describing the different hierarchies of influenza surveillance in Vietnam.
Prof Mark Jit — from Public Health England and LSTMH — giving a talk on carrying out health-economic assessments of influenza burden.

Juhye Lee — from Dr Jesse Bloom’s lab at the FHCRC — explaining how the Bloom Lab’s antigenic profiling methods can be used to determine which antigenic variants a population should select for.
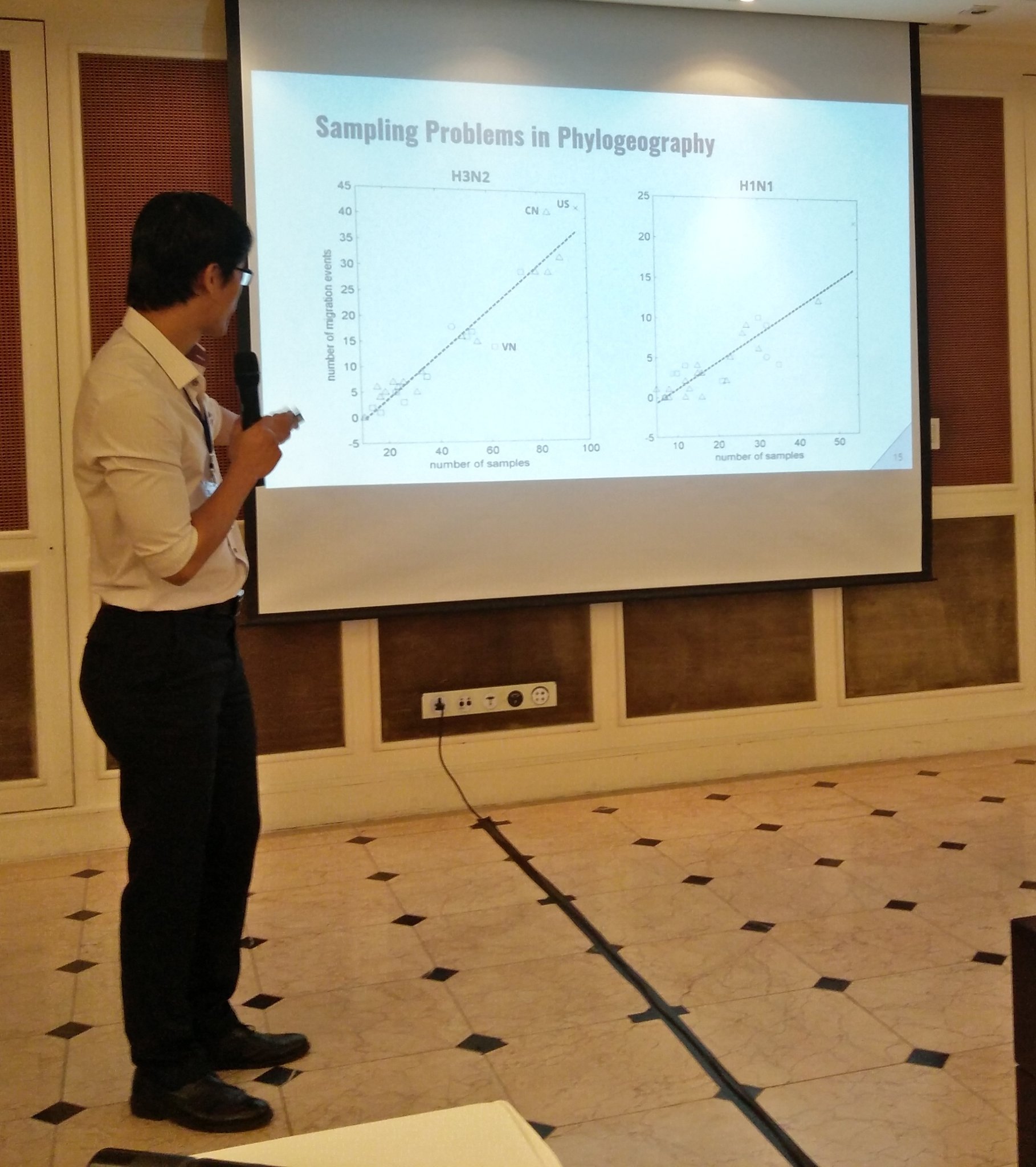
Ha Minh Lam — current Oxford DPhil student — discussing the pitfalls in phylogeographic analyses when attempting to reconstruct migratory patterns in influenza virus.

Dr Nguyen Thi Nam Lien — from Hue Central Hospital in central Vietnam — receiving an award for her heroic efforts in collecting more than 9000 general-population serum samples.

Dr Dong Thi Hoai Tam — one of the clinicians leading our work on mHealth ILI surveillance in Ho Chi Minh City.

Workshop Introduction by Maciej Boni.

Prof Le Thi Quynh Mai — vice-Director of Vietnam’s National Institutes for Hygiene and Epidemiology.

Dr Nguyen Van Vinh Chau — Director of the Hospital for Tropical Diseases in Ho Chi Minh City — and a big supporter of OUCRU’s serology and mHealth studies.

Nguyen Thi Le Thanh – study coordinator at OUCRU who did the heavy lifting on study management and administration for OUCRU’s serum bank and the community ILI mHealth study.

Pictured from left to right: Huynh Thi Phuong (molecular lab, serology lab), Nguyen Thi Le Thanh (study coordination), Maciej Boni, Nguyen Ha Thao Vy (molecular lab, serology lab).